A 42 year old male patient with HFrEF
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective, current, best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome!
CHEIF COMPLAINTS
42 yr old male electrician, came to casualty with cheif complaint of
1. SOB grade 4 , progressed from grade 3 since 4-5days
2.abdominal distension since 4-5 days
3. Bilateral pedal edema upto ankle since 4-5 days .
1yr back diagnosed as TB , used medication for 4days and stopped.
PRESENT ILLNESS
Patient was apparently asymptomatic till July 21 when he was admitted here in Kims ,nkp, with symptoms of SOB , pedal edema ,
diagnosed as HFrEF with EF= 32% , with COPD, with LEFT ULCER ON FOOT managed conservatively with diuretics, beta blockers , one episode of AF ( paroxysmal) resolved.
Patient continued to consume alcohol 15days after discharge with increased binge drinking since 10days , followed by cough, productive, no diurnal variation , associated with low grade fever and SOB , progressed to grade 4 gradually, associated with orthopnea , with abdominal distension and bilateral pedal edema upto ankle.
Not a k/c/o diabetes/ hypertension/ asthma/epilepsy.
K/c/o alcoholic 180ml whiskey/day since 20yrs .
Gutka consumption since 20yrs.
No similar complaints in the past.
Past history:
2018:
His left foot big toe got hit by iron rod during work, used pain killers but did not subside , foot got swollen the next day, he came to our hospital that day , skin flap from right thigh is grafted to his left foot. He used regular medication for given period. He was fine till 2yrs, then got diagnosed for TB , used medication only for 4days .
Now before 3months , he got admitted due to jaundice in our hospital, after admission,next day he developed ulcers on left foot ankle, treatment was being given, now again multiple ulcers were developed.
Chronic alcoholic 180ml/day whiskey since 20yrs.
Before 2018 , he was fine with his routine work life.
O/E
Patient is conscious, coherent,co operative.
Afebrile
BP: 90/60mmhg
PR- 112bpm
RESP. RATE: 34CPM
Spo2: 89% room air
CVS:
Parasternal heave +
Apex - visible, diffuse.
S1,S2 heard.
RESP.SYS:
Dyspnea- grade 4
Wheeze + , bilateral end inspiration.
Position of trachea - central
Adventitious sounds :
Rhonchi + , rales+ , in bilateral ISA .
PER ABDOMEN:
Soft,Distended.
No any tenderness.
Shifting dullness+
Bowel sounds heard.
CNS : NAD.
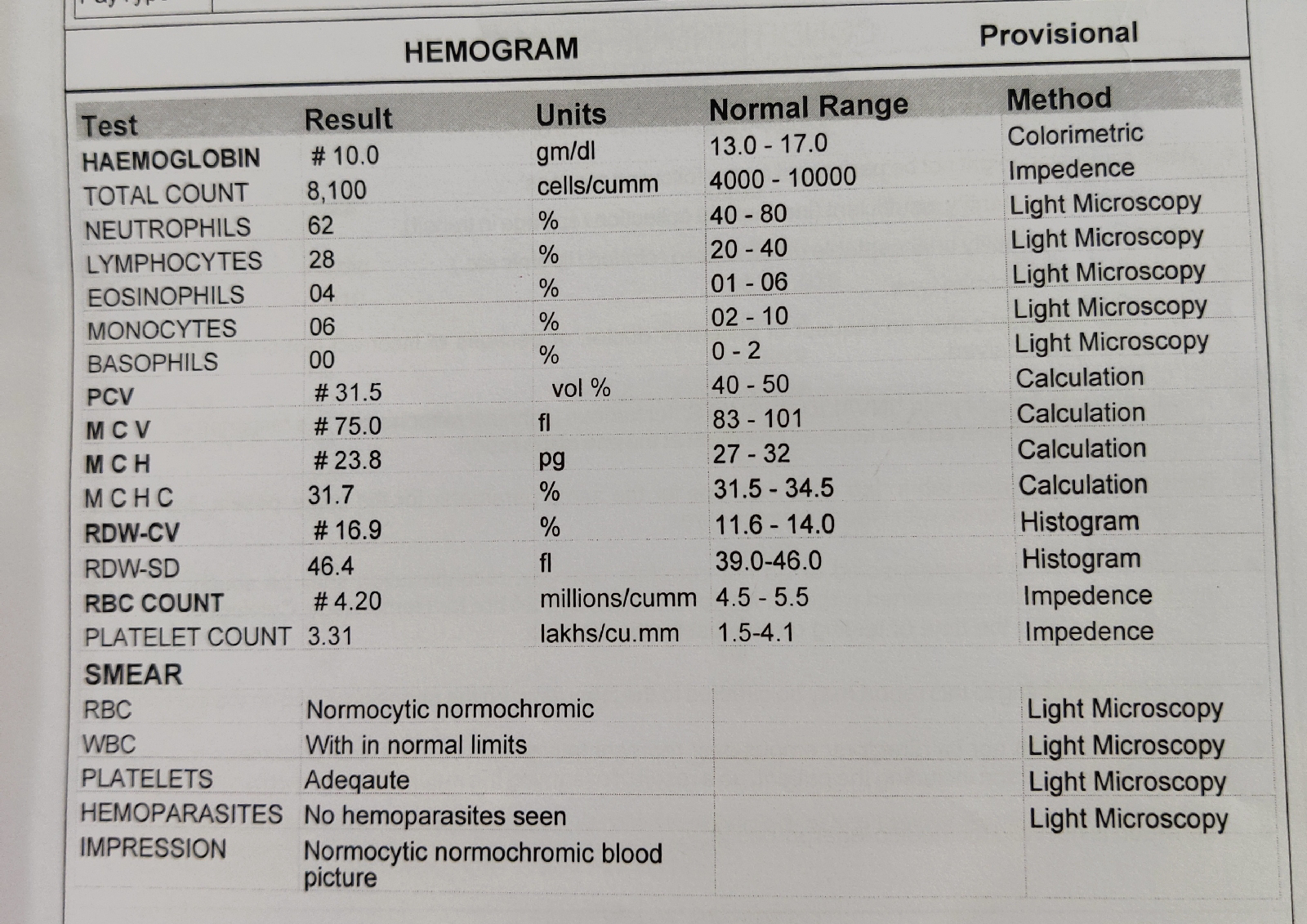
INVESTIGATIONS:
Serum creatinine: 2.1
Blood urea : 75
Serology: negative
2D ECHO:
Moderate to severe TR+ with PAH : mild MR+ , trivial AR +
Global akinetic , no AS/MS
severe LV dysfunction.
No diastolic dysfunction,
No LV clot.
PROVISIONAL DIAGNOSIS:
HFrEF with EF=27% ? Beri Beri
With h/o paroxysmal AF (resolved)
With Right sided pleural effusion
with h/0 TB ( defaulter ) used medication for 4 days.
TREATMENT:
1. 02 Inhalation @ 4Litres/min.
2.propped up posture.
3.fluid restriction < 1liter/day
4. Salt restriction < 2gm/day
5.Inj. Lasix 40mg / i.v / TID
If SBP > 100mmhg.
6.Tab. Ecospirin-Av 75/20mg OD
7. Inj. Thiamine 3amp /i.v / in 100ml NS stat
8. Neb with IPRAVENT , DUOLIN /stat
IPRAVENT= 8th hourly
BUDECORT = 12th hourly.
9. Strict I/o monitoring.
10. BIPAP intermittently every 2hrs.
11.Foleys catheterization
12.Inj. Lasix 10amp (vials)
20ml.lasix + 30ml NS= 200mg.
1ml= 200/50= 4mg.
At 2ml/hr ( 8mg/hr).
13. T. Met Xl 25mg /po/stat
14. Inj. HYDROCORTISONE 100mg/i.v /stat
PLEURAL TAP DONE .
19/10/2021 INVESTIGATIONS:















Comments
Post a Comment